The human microbiome project was a major undertaking
by the National Institutes of Health, with a fairly simple mission: understand
the bacterial communities living in and on the human body, and the potential
impact these communities may have on health. Hundreds of individuals donated
everything from feces to nasal secretions. However, one key system was ignored -
human milk. That’s right – the microbiome of human milk was not studied.
Probably some of this had to do with a long standing
myth that human milk was sterile. Why study something without bacteria,
right? But, as we have quickly learned – human milk is far from sterile. The
average baby consuming 800 mL/27 ounces of human milk will received between
100,000 and 10,000,000 million bacteria from human milk per day (Fernandez et
al., 2013).
 |
| Figure 1: The Human Microbiome Project is not interested in milk. I fixed their image to better reflect this. |
Fortunately, research into the human milk microbiome
has continued despite this oversight by the Human Microbiome Project. It
appears that nine “operational taxonomic units” (generally closely related
species based on DNA analysis of the bacteria) are extremely common in most
mothers studied to date: Streptococcus, Corynebacteria, Bradyrhizobiaceae,
Staphylococcus, Serratia, Ralstonia, Propionibacterium, Pseudomonas, and Sphingomonas.
These nine groups typically account for more than 50% of total bacteria.
Bififobacterium and Lactobacillus are also common, but less universal
(Fernandez et al., 2013).
The microbiota of milk appears to be quite stable
(Fernandez et al., 2013), although a few factors appear to shape the
composition. First, mothers with higher BMIs (in the obese range) produce colostrum
with more Lactobacillus, and mature milk with more Staphylococcus and less
Bifidobacterium (Cabera-Rubio et al., 2012). Cabera-Rubio and colleagues (2012)
also found that greater pregnancy weight gain predicted more Staphylococcus in
the milk in a small study of 18 mothers, half obese and half of normal weight.
But here is the really neat part – guess what else
altered the milk microbiota? Type of delivery. Mothers who had caesarian
sections had a different milk microbiota than mothers who had a vaginal
delivery. And the variation continued – mothers undergoing emergency caesarians
after laboring had milk microbiotas closer to those of women who delivered
vaginally than women with elective caesarians.
Where do the bacteria come from? Initially, it was
thought that the milk microbiome was really just contamination from the skin
microbiome. However, this is WRONG, WRONG, WRONG. While the milk microbiome
does contain some of the same families of bacteria as skin, multi-site sampling
of mammary skin and milk revealed that these are not the same species and/or
genera. Instead, it appears that the microbiome of milk comes from several
places, including the maternal gut microflora. Current evidence supports
dendritic cells as the likely transfer mechanism. These cells, along with some
macrophages, can open the tight junctions between cells forming the gut barrier
and take in living bacteria. These cells can then maintain the live bacteria
for several days in mesenteric lymph nodes scattered throughout the body
(Fernandez et al., 2013). Dendritic cells are also pretty picky about what they
take up – dead bacteria or latex beads will not activate immature dendritic
cells for bacteria uptake, while commensal species, like Lactobacillus, show
high levels of binding (Rescigno et al., 2001).
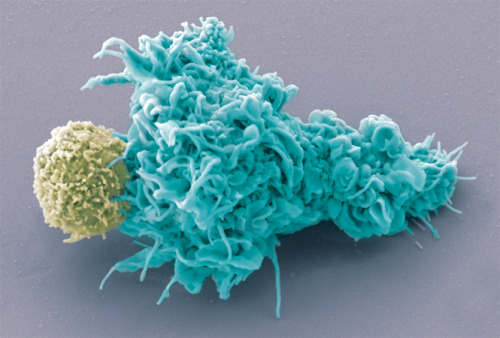 |
| Figure 2: Dendritic cell (shown in blue). Image from http://www.cell.com/pictureshow/immunology |
This allows for oral manipulation of the milk
microbiome – mothers given supplemental Lactobacillus from three strands, L. gasseri, L. fermentum, L. salivarius,
showed transfer of these strands to the milk (Jimenez et al., 2008).
This lead to the logical question – could these
strands be used to treat mastitis? Arroyo et al., (2010) randomized 352 women
with mastitis to three groups – one dosed with L. fermentum, one dosed with
L. salivarius, and one given standard antibiotic treatment (4 different
drugs were used). Bacterial counts for milk were obtained for all mothers on
Day 0 – that is before treatment started. All mothers had bacterial counts of
4.35-4.47 log10 CFU (colony forming units) – a little less than double the
recommended bacterial counts for milk of 2.5 log10 CFUs. Mothers received 21
days of treatment, and milk bacterial counts were repeated on day 21. Women who
received L. fermentum had mean
bacterial counts of 2.61 log10 CFUs; L.
salivarius had bacterial counts 2.33 log10 CFUs with clinical relief of
mastitis, and all reported reductions in reported breast pain. Mothers who
received antibiotics did not fare as well. Mean bacterial count for antibiotic
receiving mothers was 3.28 log10 CFUs and pain scores were much higher. Three
months later, only 8.8% of mothers receiving either L. fermentum or L. salivarius had experienced recurrent mastitis,
while 30.1% of mothers receiving antibiotics had. All differences between
antibiotic and probiotic groups were significantly different – the kind of significant
difference that makes researchers do their happy dance.
Figure 3: This is how I picture the researchers after making this discovery - just substitute a computer for the piano. Gif by PEANUTS.
So the milk microbiome appears to be protecting
mothers – but there is also good evidence that it is protecting infants. Little
is known about the salivary microbiome of infants, but based on preliminary
evidence, it appears to, not surprisingly, have some overlap with the milk
microbiome (Nasidze et al., 2009). The milk microbiome also appears to
contribute to the microbiome of the infant GI tract, as well as the development
of immune function in the infant (Fernandez et al., 2013). Infants supplemented
with Lactobacillus fermentum (yes,
the same as used for the treatment of mastitis) showed significant reductions
in diarrheal and respiratory infections in early infancy compared to control
infants (Maldonado et al., 2012). Many of the bacteria in the milk microbiome
are protecting both the mother and the infant from infection, and may even be
involved in the development of immune tolerance.
Milk remains amazing – even the bacteria in milk!
References
Arroyo
R, Martín V, Maldonado A, Jiménez E, Fernández L, Rodríguez JM. (2010) Treatment
of infectious mastitis during lactation: antibiotics versus oral administration
of lactobacilli isolated from breast milk. Clinical
Infectious Diseases 50:1551–8.
Cabrera-Rubio
R1, Collado MC, Laitinen K, Salminen S, Isolauri E, Mira A. (2012) The human
milk microbiome changes over lactation and is shaped by maternal weight and
mode of delivery. Am J Clin Nutr. 96(3):544-51.
Fernández
L1, Langa S, Martín V, Maldonado A, Jiménez E, Martín R, Rodríguez JM. (2013) The
human milk microbiota: origin and potential roles in health and disease. Pharmacol Research 69(1):1-10.
Jiménez
E, Fernández L, Maldonado A, Martín R, Olivares M, Xaus J, et al. (2008) Oral administration
of lactobacilli strains isolated from breast milk as an alternative for the
treatment of infectious mastitis during lactation. Applied and Environment Microbiology 74:4650–5.
Maldonado
J, Ca˜nabate F, Sempere L, Vela F, Sánchez AR, Narbona E, et al. (2012) Human
milk probiotic Lactobacillus fermentum CECT5716 reduces the incidence of
gastrointestinal and upper respiratory tract infections in infants. Journal of Pediatric Gastroenterology and
Nutrition 54:55–61.
Martín
R, Olivares M, Marín ML, Fernández L, Xaus J, Rodríguez JM. (2005) Probiotic potential
of 3 lactobacilli strains isolated from breast milk. Journal of Human Lactation 21:8–17.
Nasidze
I, Li J, Quinque D, Tang K, Stoneking M. (2009) Global diversity in the human salivary
microbiome. Genome Research 19:636–43.
Rescigno
M, Urbano M, Valzasina B, Francolín M, Rotta G, Bonasio R, et al. (2001) Dendritic
cells express tight junction proteins and penetrate gut epithelial monolayers
to sample bacteria. Nature Immunology
2:361–7.